We should all face the fact that oncology care is complicated. Nothing can sugarcoat it. And, adding the rising cancer rates worldwide, we can only imagine what kind of pressure oncology teams handle every single day.
As of 2022, specialists diagnosed approximately 20 million new cancer cases, with the prediction for the number to increase by about 77% by 2050.
Massive data sets, multi-step treatment plans, patient records, pathology data, dozens of specialists, lab tests, imaging, and so on and so far. What I can say is that oncology doctors are already handling more than they can. Hopefully, one day, someone will find a cure or vaccine to save us from this intimidating disease. But what can be done now? That’s where AI steps in.
When I mention oncology AI solutions, I don’t mean some flashy tools or sci-fi fantasy. They are real game-changers that are already taking over daily tasks in hospitals. You may be wondering how it’s even possible? Well, they help clinicians work smarter by reducing administrative hassle, speeding up data analysis, coordinating multidisciplinary groups, automating follow-ups, and providing real-time clinical insights. Doctors benefit the most as they can make better decisions and focus on actually helping patients instead of doing paperwork.
AI and oncology can work hand-in-hand, improving the accuracy and efficiency of CAD, enhancing diagnostics through the integration of imaging, histology, genomics, and EHRs, perfecting screening, early diagnosis, and predictive modeling, and, in general, boosting accuracy in detecting cancer. Moreover, according to PubMed Central, AI shows great results in detection accuracy, with breast cancer achieving over 96% accuracy, lung cancer showing 87% specificity, prostate cancer demonstrating an AUC of 0.91 compared to radiologists' 0.86, and colorectal cancer achieving 97% sensitivity and 95% specificity.
My goal in this article is to give a clear picture of the benefits, challenges, implementation considerations, and key cases, with our own included. Ready to learn more and see AI agents in action? Let’s explore.
The Current Challenges in Oncology Workflows
When I say that oncology is complex, I mean it is really complex. There are piles and piles of data clinicians must juggle. On top of that, there are many patients waiting endlessly, and medical professionals running between multiple systems. And all of them would like to move as fast as possible. But what are the bottlenecks? Let’s break them down.
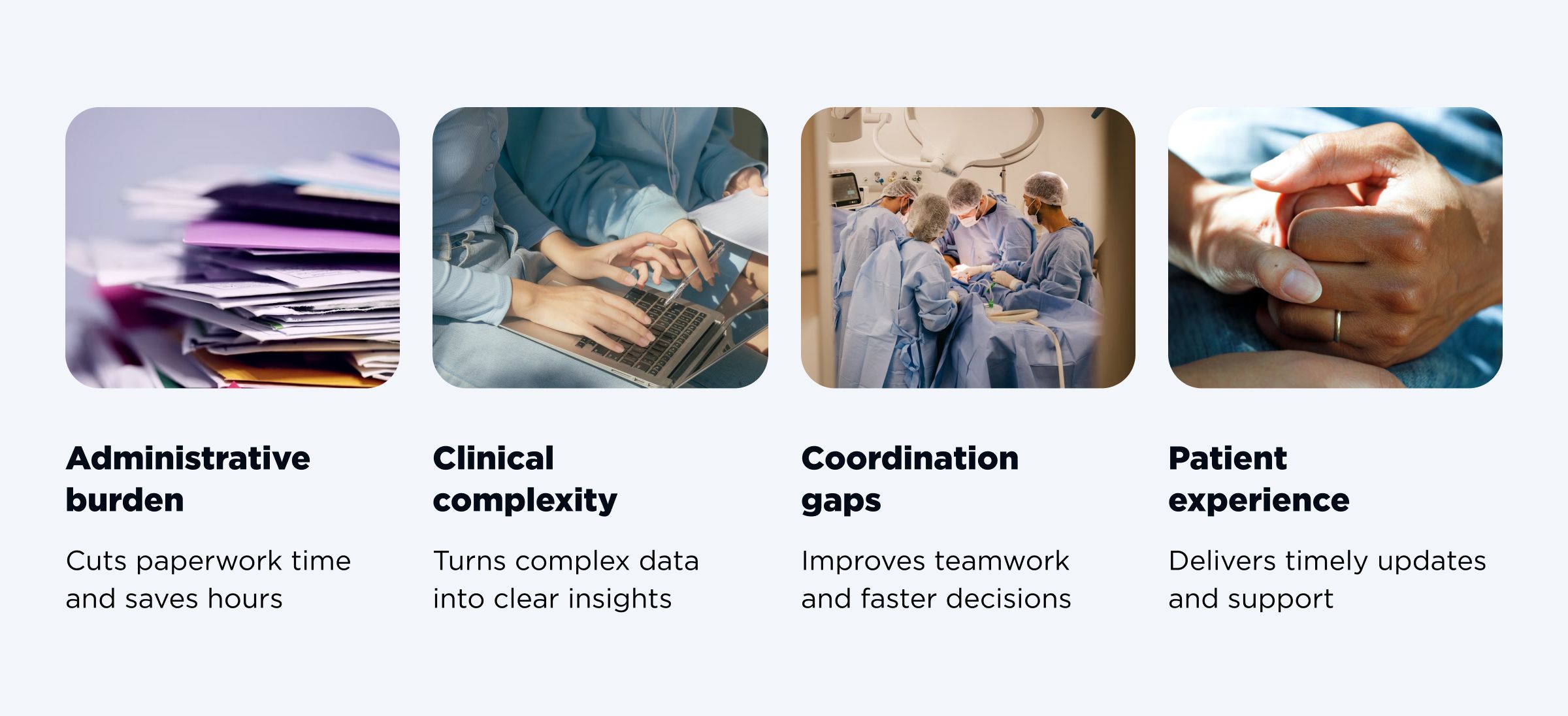
- Administrative burden
Hours and hours are spent doing manual data entry, recording fragments of patient data, chasing lab reports, and filling preauthorization forms. In my humble opinion, that’s a lot of precious time taken away from patient care. AI in oncology workflows can definitely solve this issue of spending so much time on administrative tasks, tumor board meetings, and paperwork. - Clinical complexity
Oncology is a web, and a difficult one to navigate through. Moreover, there’s no one-size-fits-all cancer treatment. Medical professionals need to interpret numerous documents like pathology reports, genomic sequencing, prior therapies, treatment options, imaging data, and always-updating clinical guidelines. It is just mentally exhausting, error-prone, and cognitively heavy to efficiently consider all these nuances. - Coordination gaps
I will not be exaggerating when I say that there are many teams involved in the whole oncology workflow. Tumor boards, multidisciplinary teams (MDTs), oncologists, radiologists, pathologists, surgeons, pharmacists, nurses, and the like. Everyone involved must be on the same page. Just imagine the number of appointed meetings, shared notes, confirmed schedules, aligned treatment plans, and multiple follow-ups needed for proper care. - Patient experience
What is a common experience of oncology patients (unfortunately)? Delayed results, long waits, fragmented communication, rare personalized treatment plans, and inconsistent updates. When such patients feel uncomfortable and anxious, it can also affect the outcomes of the treatment. Thanks to AI in oncology, they can get timely information, personalized updates, and reassurance that their medical care team is well-coordinated.
I know that oncology workflows are a mix of high stakes, heavy workloads, and fragmented data. However, when AI comes into the game, everyone gets better accuracy, higher efficiency, and speed.
Key Use Cases of AI Agents in Oncology
Considering all the current challenges that need to be handled, let’s make it clear - oncology AI solutions are practical and make an impact. There are many tools available. However, I’d like to highlight the most common and key use cases in oncology.
| Automated patient triage | Clinical decision support | Workflow orchestration | Imaging and pathology | Research and trial matching |
| Intake form analysis, risk stratification, and prioritization of urgent cases | Summarizing cases, recommending guideline-based therapies, predictive models for survival rates, and treatment response | Scheduling coordination across radiology, chemotherapy, and surgery, as well as automated follow-up reminders and patient engagement messaging | AI-powered image recognition for tumor detection and automated pathology report summarization | Identifying eligible patients for clinical trials in real time |
Automated patient triage
AI agents can analyze patient data, flag high-risk patients and cases, and prioritize urgent situations. It’s about handling first patient interactions. What are the key tasks this system performs?
- Parsing patient-reported symptoms;
- Identifying high-risk oncology markers;
- Prioritizing urgent consultations.
Clinicians don’t need to manually sort all reports or worry about missing critical cases. I would describe it as a virtual triage nurse that can quickly scan data, detect concerning lab trends, and alert the oncology team. As a result, it reduces delays and eliminates oversights.
Clinical decision support
As I’ve mentioned a couple of times, AI doesn’t replace oncologists but empowers them. Tumor boards are where high-stakes decisions happen. That is why they need data. However, there’s so much data that it can become overwhelming. This is when AI oncology agents step in. They can:
- summarize patient cases with structured and evidence-backed insights,
- suggest guideline-based, latest treatment options,
- run predictive models to estimate survival rates or treatment outcomes.
Briefly speaking, they become smart assistants that digest and process all the relevant data in a matter of seconds. As a result, clinicians can focus on human-related decisions that really matter with more precision, detail, and information.
Workflow orchestration
Scheduling in oncology is a mess, if not a nightmare. There are so many aspects to align with. Coordinating scans in radiology, chemo, surgeries, and constant follow-ups. Good news, AI can help here as well! Various solutions can:
- automate coordination,
- sync appointments,
- send reminders to patients and for follow-ups,
- suggest optimal times based on treatment protocols and doctors' availability.
Such assistants never sleep and always make sure everyone is on the same page.
Imaging and pathology
Imaging and pathology can benefit significantly from AI implementation. Why is it such a game-changer?
- AI-powered image recognition can flag tumors, detect suspicious areas in scans, and see what the human eye may sometimes miss.
- AI solutions can summarize complex pathology reports, highlight key findings, and stage information.
- Clinicians are involved in reviewing results. However, AI significantly accelerates diagnostics and eliminates the risk of missing out on something.
The bottom line, such AI use cases speed up the process with better accuracy and more details.
Research and trial matching
It might be challenging to find eligible patients. Oftentimes, this process is slow and manual. I think you know where I’m leading. You might be right because AI can identify eligible patients in real time.
- AI scans EMR data, genomic information, and trial criteria.
- The platform matches patient profiles with clinical trial eligibility criteria.
- Patients are identified without manual review.
As a result, no patient profile is missed, it opens new treatment opportunities, and speeds up research progress. It is a win-win approach for medical innovation and patients.
Discovering Benefits of Implementing AI Agents
As you can see from the examples of use cases, the benefits of AI for oncology are invaluable. Moreover, the results we can experience from smart AI integration are tangible, not just theoretical. As there are measurable advantages to the oncology industry, let me break down what is in it for hospitals, patients, and clinicians.
| Benefits | What they bring |
| Efficiency gains | AI reduces administrative workload for medical professionals. |
| Accuracy and consistency | AI implementation leads to lower error rates in diagnosis and documentation. |
| Speed to treatment | Thanks to AI agents, the turnaround time for care plans and diagnostics speeds up. |
| Better outcomes | There’s better and data-driven personalization of treatment plans and results. |
| Cost optimization | Due to better resource allocation, costs are reduced as no test duplications are made. |
- Efficiency gains
Thanks to AI oncology solutions, clinicians spend much less time on documentation, administrative tasks, and paperwork in general. On the other hand, they can devote more time to working with patients. I must note that efficiency gains play a significant role in making meetings smoother, documentation automated, and preauthorization forms generated easily. - Accuracy and consistency
Let me explain how AI agents work. They pull data directly from EMRs and validate everything using a rule-based approach. This way, AI reduces errors in reporting, diagnosis, treatment planning, and documentation. Such an automated extraction and summarization always leads to fewer human errors. - Speed to treatment
I always say that AI is here to speed us up. AI in oncology is no exception. However, it’s not about “time to market” but “time to treatment”. Thanks to faster turnaround on imaging, labs, and multidisciplinary approvals, patients can get a chance to start their treatments sooner. I hope you understand what it means for the outcomes. - Better outcomes
Speaking of outcomes, that is another benefit brought about by oncology AI solutions. It’s not only about speed and accuracy, but also about data-driven personalization. By analyzing and using insights, AI can help personalize therapy for each patient. This allows for treatment plans to align with specific factors, from genomics to comorbidities. - Cost optimization
I’ve seen cases when oncology workflows, managed only by humans, kept duplicating tests. Thanks to smart AI-powered automation, there are fewer (or no) duplicated tests, smarter resource allocation, and fewer delays. Altogether, it saves the healthcare system a lot of money. At the same time, it reduced the burden on oncology patients.
What is the bottom line? These are just the main benefits I wanted to share with you. As you can see, AI for oncology is like a never-tiring assistant amplifying human precision and efficiency. It is a great collaboration for everyone involved: patients, medical professionals, hospitals, and the healthcare industry as a whole.
Implementation Considerations
I know it very well that deploying AI for oncology isn’t a plug-and-play case. Hospitals must think strategically and keep essential things in mind.
- Data readiness
EMR data must be clean, structured, and interoperable. AI works best with high-quality data. - Integration
There are existing hospital systems and workflows. The platform should fit seamlessly without disrupting anything. It means AI agents have smooth EMR integration, secure APIs, and minimal friction for medical professionals. - Regulatory compliance
It is non-negotiable for AI platforms to comply with HIPAA, GDPR, PHI protections, and other local or privacy-specific regulations. AI-powered systems must ensure auditability. - Change management
In order to trust AI tools and their outputs, medical professionals need training and technical confidence. Human-in-the-loop (HITL) approaches are helpful in this matter as every recommendation is reviewed by clinicians before being written into EMRs. - Ethical AI
Explainability, transparency, and bias mitigation are vital. They make sure that the platform helps without causing any unintended harm. And clinicians should also understand why AI suggests that or another treatment or flags some high-risk patients.

Improve healthcare workflows with AI
CONTACT USCase Study: AI Agent Platform for Oncology Workflows
To better understand the implementation process, I’d like to show what AI in oncology really looks like in real life in this section of the article. This case study by OTAKOYI describes how a top-notch AI agent can transform the whole oncology workflow. Let’s explore more.
Executive summary
The main goal was clear: to make oncology workflows smarter, safer, and faster. Our team designed it with a standards-first approach, so it integrates directly with EMRs and delivers bi-directional read/write, data exchange, real-time support, and automated preauthorization workflows.
The best thing about this platform is that it captures live discussions from the meetings, extracts key medical terms, drafts clinical notes, and generates FHIR resources for preauthorization. What is more, it is done under strict PHI governance and HITL (human-in-the-loop) controls. It is an essential feature as clinicians remain in charge of all decisions with ensured safety, improved accuracy, and strict accountability.
The problem faced
There’s endless data exchanged across systems. Imaging, pathology notes, lab reports, genomic sequencing, previous treatments, and even external medical resources. It is not so easy to collect all the data from MDT (multidisciplinary team) and tumor board meetings. So, the oncology team faced the key challenges as follows.
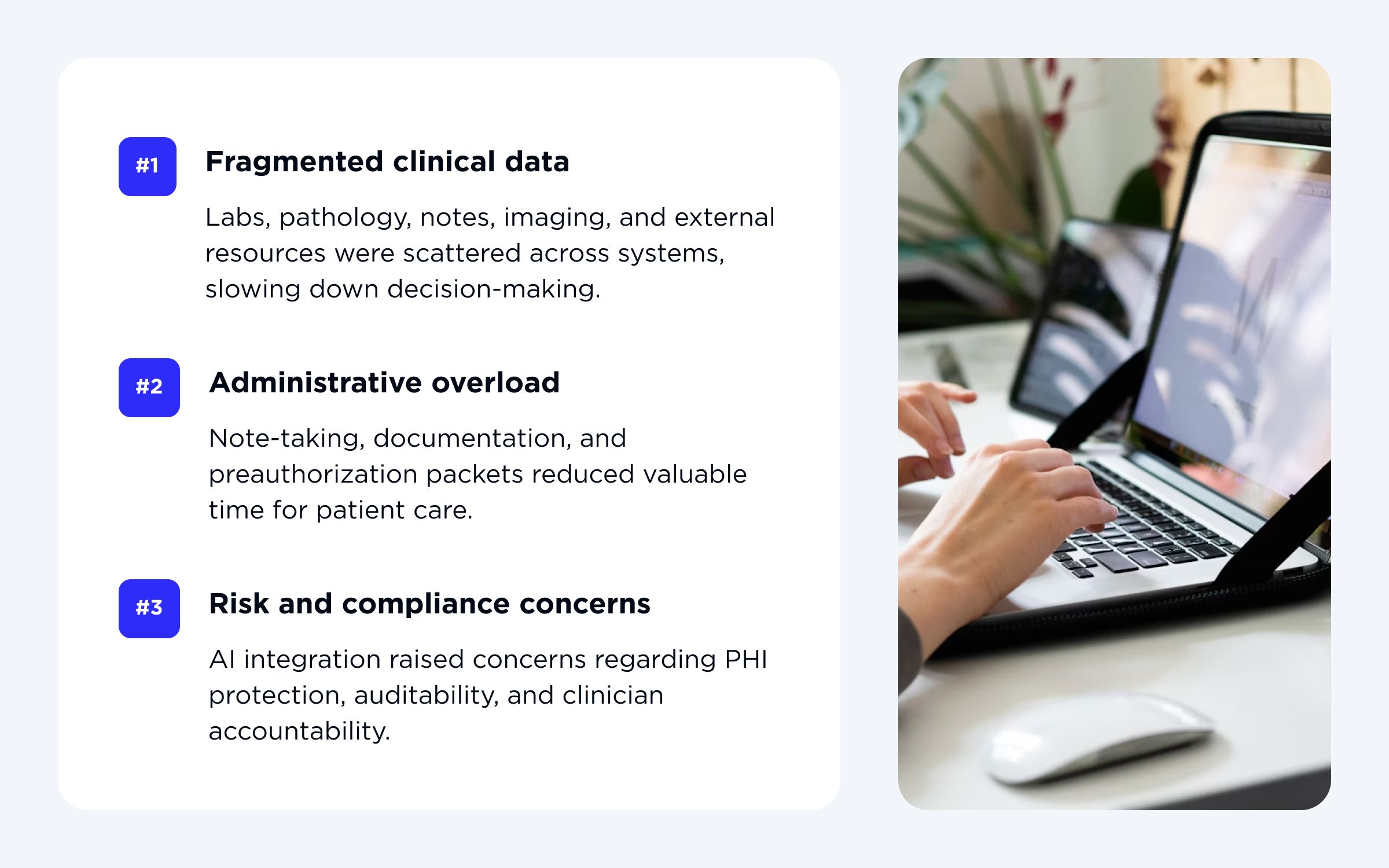
- Fragmented data was slowing down the whole decision-making process. Doctors had to spend too much time searching for information across systems manually.
- There was too much paperwork involved, which is an administrative overload. Clinicians would lose a lot of valuable time on taking notes, documentation, and preauthorization packets.
- Implementing AI in oncology workflows raised legitimate concerns regarding data protection, clinical accountability, and auditability. Compliance and risk were real challenges.
Objectives
As follows from those three key challenges, our team wanted to make sure the AI agent can tackle them. That is why the primary objectives were:
- Reduce administrative load and time spent during MDT and tumor board meetings, and simplify documentation in general.
- Provide accurate and context-aware clinical summaries as well as draft candidate orders for doctors to easily review and approve.
- Design an interoperable system that can integrate with multiple EMRs and scale easily. At the same time, it must ensure robust PHI security, compliance, and audit controls.
The team didn’t want to reinvent oncology care but to make it faster, easier, and more accurate by adding a tool that works behind the scenes.
Solution overview
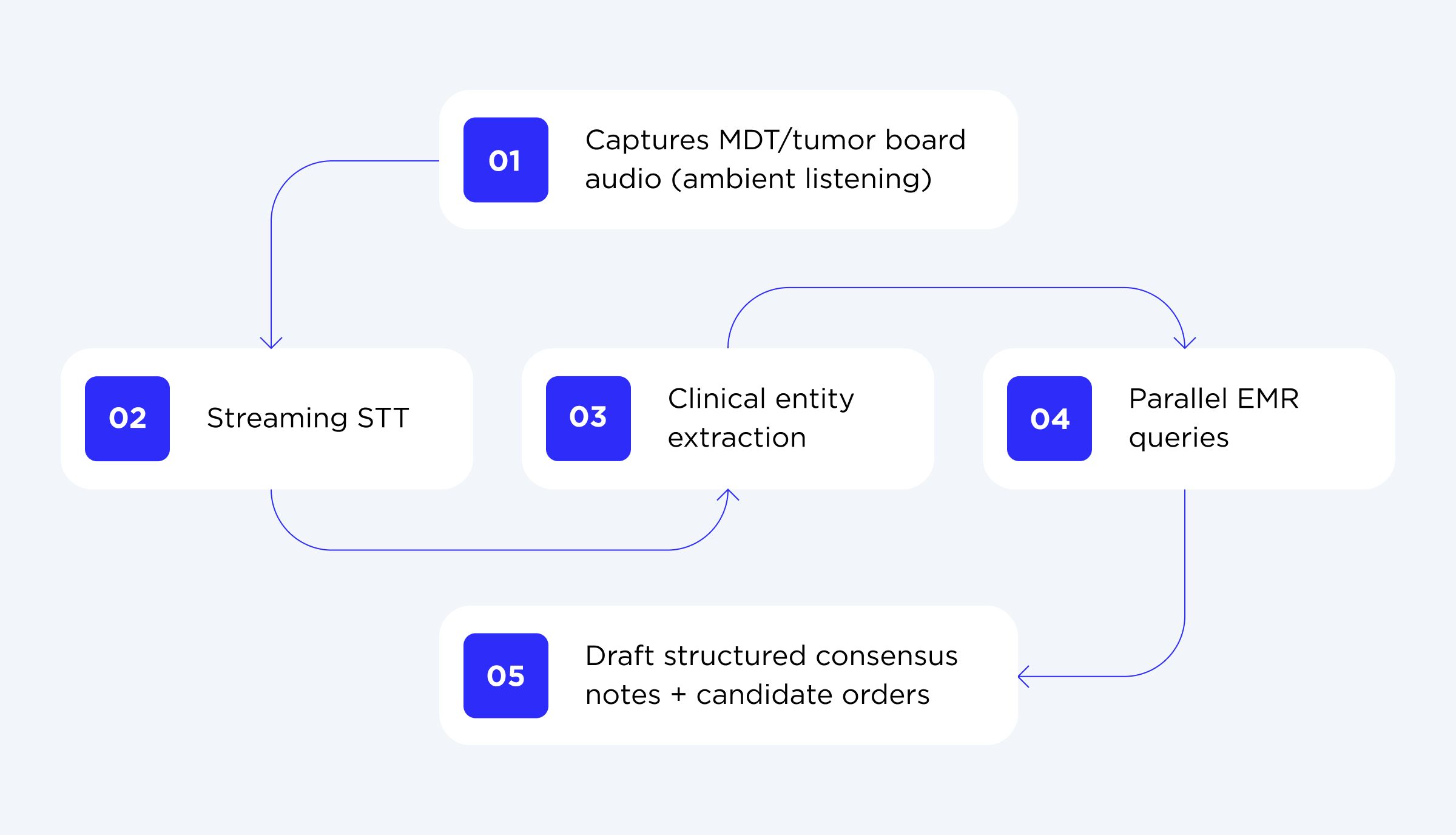
To make it simpler to understand how it works in practice, let me guide you through the solution logic.
- EMR integration
First of all, the platform uses modular and standards-based architecture that connects to EMRs (Epic, Cerner, and others) through SMART-on-FHIR and HL7 protocols. It makes it possible for the AI agent to read all the necessary oncology data and write clinician-approved notes, orders, and communications in real time. - Data capture
Moreover, during MDT and tumor board meetings, it captures ambient audio and converts it to a structured text via STT (speech-to-text). - Clinical data extraction
Following data capture, it extracts clinical entities like diagnoses, medications, treatment options, and staging. - Parallel EMR queries
In parallel, the system runs other tasks. It can retrieve relevant EMR data like labs, imaging, pathology, previous therapy, prior reports, and structured oncologic data. - Draft generation
After all previous steps, AI creates consensus notes and candidate orders. Note: they are packaged as FHIR resources for preauthorization. - Human oversight
All outputs generated by the AI agents are reviewed, edited, and attested by clinicians before anything is committed to EMR. This is about full human oversight (HITL). - Preauthorization
As mentioned, all drafts are packaged as FHIR resources (ServiceRequest, DocumentReference) for preauthorization and/or payer submission.
EMR integration
To put it simply, the AI agent gets the data directly from the EMR. It includes all the needed data: problem lists, medications, allergies, lab and imaging reports, pathology findings, prior visit notes, and structured oncologic data.
In technical terms, the platform is vendor-agnostic and connects with Epic, Cerner, and other EMR systems through SMART-on-FHIR and HL7 adapters, with additional vendor-specific adapters managed under a unified capability layer. The full integration through Epic’s App Orchard or Cerner CODE isn’t finalized yet. However, the team is actively evaluating different integration stacks (e.g., LangGraph + LangChain + custom tools or LangGraph + MCP combinations).
We aimed to ensure low latency. That is why the architecture supports session prefetching, parallel API calls, and streaming partial outputs. The result? Clinicians can see early drafts even while deeper research is finishing up in the background.
Through such a tight integration, the platform has become an integral part of the hospital’s workflow. To summarise, let’s break down what it reads and writes.
- Reads: problem lists, medications, allergies, labs, imaging, pathology, prior visit notes, structured oncologic data.
- Writes (post-attestation): consensus notes, clinician-approved orders, referrals, patient-portal communications.
Security and governance
Oncology data is always about sensitive information. That is why our team built the platform with privacy and compliance in mind and at its core. Let’s explore it in more detail.
- PHI protection
Middleware pseudonymizes identifiers and transforms free text into structured JSON. - Scoped API access and OIDC tokens
Due to SMART-on-FHIR and OIDC tokens, the AI operates on the least-privilege access per task, meaning it views what is strictly necessary for each task. - Audit and monitoring
There’s full EMR-to-AI logging monitoring (via AWS CloudTrail, CloudWatch, LangSmith) and anomaly detection (through GuardDuty and Security Hub). - Incident response
There’s automatic credential revocation, service isolation, and formal client notification within regulatory windows. - HITL safeguards
No AI output can enter EMR or be committed without clinician review first. - Cloud and orchestration
The platform runs on robust AWS services (Bedrock, Transcribe Medical, Comprehend Medical, EKS/ECS Fargate). Meanwhile, orchestration is handled by LangGraph + MCP, with optional LangChain or custom tooling. - Compliance
The system is completely compliant with HIPAA, GDPR, and HL7 FHIR R4 security standards. - Access control
Role-Based Access Control (RBAC) governs user access. Sessions automatically expire to prevent any threat. - Data encryption
All the data (at rest and in transit) is protected by AES-256 encryption and TLS 1.3 protocols. This way, all sensitive data stays secure.
Performance and reliability
To keep workflows fast, precise, and dependable, the system is engineered for high availability and low latency:
- The system is reliable, fast, and accurate.
- Session prefetching and short-lived caching reduce repeated EMR calls.
- Due to parallelized EMR adapters, we were able to minimize latency and payload size.
- Streaming responses display partial notes early while background queries continue finishing up.
- Implementation of hybrid retrieval. It comprises domain-trained Hugging Face embeddings + keyword/metadata filters + cross-encoder reranking. This approach ensures relevant data appears first and always shows precise results.
- Automated rule-based validation is about checking schema, contraindications, and formatting before clinician review.
- Interactive latency means interactive responses under 3 seconds (even during live MDT sessions).
Example of MDT/tumor board flow
As you have become acquainted with all specifics and performance approach, let me present an example of how a tumor board or MDT session flow happens.
- Clinician opens patient context in EMR.
- AI prefetches oncology summaries, labs, imaging, prior therapies, etc.
- In real-time streaming, ambient audio capture starts.
- STT (speech-to-text) converts the whole dialogue into a structured text.
- Clinical entity extraction identifies the key terms (diagnoses, staging, and treatment plans)
- Meantime, parallel EMR queries retrieve additional supporting data (if needed).
- AI agent drafts well-structured consensus notes and candidate orders.
- Afterward, the clinician reviews, edits, and attests outcomes (HITL).
- All the approved data is committed and written back to EMR.
- Preauthorization resources are sent to utilization management or payers.
As you can see, the process is rather simple, but it saves oncology clinicians tons of precious time.
Feedback and ongoing improvement
Our team is providing continuous maintenance and support to perfect and improve the platform.
What does it include?
- In-app clinician feedback (context-linked comments, short surveys, editing metadata).
- Governance loop (with the feedback received, it prioritizes backlog for clinical and product review).
- Iterative improvements enhance and refine retrieval heuristics, UI wording, and order templates.
What are the results?
As you can see, the results speak for themselves:
| Result | Impact |
| Reduced time for paperwork | Now, clinicians have more time to focus on discussions, not writing down notes. |
| Faster and more informed decisions | Medical professionals get EMR data, imaging, and prior therapies in one view. |
| Improved patient experience | All follow-ups happen faster, and it reduces treatment initiation times. |
| Security, compliance, and transparency | AI will never replace human oversight, but it works as a trustworthy assistant. |
Key takeaway
As you can see from this case study by OTAKOYI, AI can do more than just process data. This platform proves how AI-driven tools can streamline care, empower clinicians, and ensure systems are protected. AI and oncology can go hand in hand with precise oncology workflows and efficient processes. The main advantage is that medical care becomes completely patient-centered.

Ready to build AI that understands and transforms oncology workflows?
CONTACT USWrapping Up: Advanced AI Agents in Oncology
Since you’ve reached this far, you are well aware of how powerful and useful AI tools in oncologic processes are. Of course, AI makes everything faster, smarter, more efficient, and precise. However, it isn’t its real value. AI, in this case, is a bridge between complex medical data and people who make life-changing decisions.
What would I recommend to you? First of all, make sure to rely on a dedicated software team like OTAKOYI that can implement something like their case study for your medical institution. Make sure to pay attention to all challenges, considerations, and implementation nuances. As long as AI is designed thoughtfully, with robust security and compliance standards, you can have a trusted tool to help your doctors act sooner and care deeper. Is anything more important in oncology? Every minute counts, so don’t delay!